Bone Marrow Health and Nutritional Recommendations

Bone marrow nutrition facts – Maintaining healthy bone marrow is crucial for overall well-being, as it’s responsible for producing blood cells essential for oxygen transport, immune function, and blood clotting. A balanced diet plays a vital role in supporting this critical function, providing the necessary building blocks for optimal bone marrow health. Nutritional deficiencies can significantly impair bone marrow activity, leading to various health complications.
The Interplay Between Bone Marrow Health and Nutritional Status
Bone marrow’s ability to produce healthy blood cells is directly influenced by the nutrients available to it. A diet lacking in essential vitamins, minerals, and other micronutrients can lead to reduced blood cell production, potentially resulting in anemia, weakened immunity, and increased susceptibility to infections. Conversely, a diet rich in these nutrients supports robust bone marrow function and a healthy hematopoietic system.
For example, individuals with severe nutritional deficiencies, such as those experiencing prolonged malnutrition, often exhibit impaired bone marrow function and reduced blood cell counts.
Key Nutrients for Healthy Bone Marrow Function
Several key nutrients are critical for maintaining healthy bone marrow function. These include:
- Iron: Essential for hemoglobin production, crucial for oxygen transport in red blood cells. Iron deficiency leads to anemia, a condition directly impacting bone marrow function.
- Vitamin B12: Plays a critical role in DNA synthesis and cell division, vital for the maturation of red blood cells in the bone marrow. Deficiency can cause megaloblastic anemia.
- Folate (Vitamin B9): Another crucial nutrient for DNA synthesis and cell division, essential for preventing neural tube defects and supporting healthy red blood cell production.
- Vitamin C: An antioxidant that protects cells from damage and aids in iron absorption, both of which are crucial for optimal bone marrow function.
- Copper: A cofactor in several enzymes involved in iron metabolism and red blood cell formation. Copper deficiency can lead to anemia.
Dietary Recommendations for Optimal Bone Marrow Health
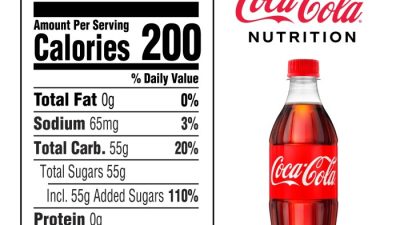
A balanced diet rich in a variety of nutrient-dense foods is the cornerstone of supporting healthy bone marrow. This includes consuming plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limiting processed foods, sugary drinks, and excessive alcohol consumption is also essential. Regular physical activity and maintaining a healthy weight also contribute positively to overall health, including bone marrow function.
Foods Rich in Nutrients Beneficial for Bone Marrow
The following list categorizes foods rich in nutrients essential for supporting healthy bone marrow:
Iron-Rich Foods:
- Red meat (beef, lamb)
- Dark leafy green vegetables (spinach, kale)
- Legumes (beans, lentils)
- Fortified cereals
Vitamin B12-Rich Foods:
- Animal products (meat, poultry, fish, eggs, dairy)
- Fortified plant-based milks and cereals
Folate-Rich Foods:
- Dark leafy green vegetables (spinach, kale)
- Legumes (beans, lentils)
- Citrus fruits
- Fortified grains
Vitamin C-Rich Foods:
- Citrus fruits (oranges, lemons)
- Bell peppers
- Strawberries
- Broccoli
Copper-Rich Foods:
- Shellfish (oysters, crab)
- Nuts and seeds
- Legumes
- Dark chocolate
Bone Marrow Transplantation and Nutritional Considerations

Bone marrow transplantation (BMT), a life-saving procedure for various hematological malignancies and other diseases, presents significant nutritional challenges for patients. The intense treatments involved, coupled with the body’s compromised immune system, necessitate a carefully planned nutritional strategy throughout the entire process – pre-transplant, during transplantation, and post-transplant – to support healing and minimize complications.
Bone marrow is surprisingly rich in nutrients, offering a good source of iron and various vitamins. For a contrasting perspective on nutrient profiles, consider checking out the nutrition facts of a cutie , which highlights the nutritional makeup of a different food entirely. Returning to bone marrow, its high fat content also contributes to its caloric density, making it a significant energy source.
Nutritional Challenges During Bone Marrow Transplantation
Individuals undergoing BMT face a multitude of nutritional challenges. The high-dose chemotherapy and radiation therapy used to prepare the body for the transplant often cause severe mucositis (inflammation of the mucous membranes), nausea, vomiting, diarrhea, and loss of appetite (anorexia). These side effects can lead to significant weight loss, malnutrition, and compromised immune function, hindering the body’s ability to fight infection and recover from the procedure.
Additionally, the transplant itself can further suppress the immune system, increasing the risk of infections and complications, thus emphasizing the critical role of proper nutrition. Specific nutrient deficiencies, such as reduced protein intake, can further exacerbate the situation, delaying recovery and increasing morbidity.
Dietary Needs During Pre-transplant, Transplant, and Post-transplant Phases
Nutritional support is crucial across all phases of BMT. The pre-transplant phase focuses on optimizing nutritional status to improve the patient’s ability to withstand the rigors of the procedure. This involves ensuring adequate calorie and protein intake to maintain weight and muscle mass. During the transplant phase, the focus shifts to managing side effects and providing easily digestible, nutrient-dense foods.
Finally, the post-transplant phase requires continued nutritional support to aid in recovery, promote immune reconstitution, and prevent complications. A tailored approach is crucial, considering individual patient needs and tolerances.
Role of Nutritional Support in Minimizing Side Effects and Promoting Recovery, Bone marrow nutrition facts
Adequate nutrition plays a vital role in mitigating the side effects of BMT and accelerating recovery. Sufficient protein intake supports tissue repair and immune function. Adequate calorie intake prevents weight loss and maintains energy levels. A balanced intake of vitamins and minerals supports overall health and strengthens the immune system. Specialized nutritional support, such as parenteral nutrition (intravenous feeding) or enteral nutrition (tube feeding), may be necessary in cases of severe malnutrition or inability to consume sufficient nutrients orally.
This approach helps minimize complications, reduce hospital stays, and improve overall patient outcomes.
Designing a Meal Plan for Bone Marrow Transplantation
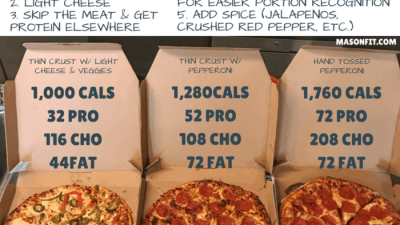
A successful meal plan for a BMT patient must balance nutrient density with ease of digestion. Small, frequent meals are often better tolerated than large ones. Foods should be soft, bland, and easy to chew and swallow to minimize irritation of the mouth and throat. The meal plan should also address specific nutrient needs, focusing on high-protein sources, healthy fats, and complex carbohydrates.
The following table provides a sample meal plan, which should be adapted to individual patient preferences and needs under the guidance of a registered dietitian or healthcare professional.
| Meal | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Example | Scrambled eggs with whole-wheat toast and a small portion of fruit | Chicken breast soup with whole-grain crackers, a small side salad | Baked salmon with steamed vegetables and brown rice |
| Nutrient Focus | Protein, carbohydrates, vitamins | Protein, fiber, low sodium | Protein, omega-3 fatty acids, vitamins |
| Considerations | Avoid fried foods | Choose low-sodium broth | Avoid overcooked vegetables |
Bone Marrow and Disease

Bone marrow diseases significantly impact nutritional needs, necessitating tailored dietary approaches for effective management and improved patient outcomes. The body’s ability to produce blood cells, crucial for oxygen transport and immune function, is directly linked to bone marrow health. Compromised bone marrow function, due to various diseases, leads to altered nutritional requirements and necessitates careful dietary intervention.Nutritional strategies in managing bone marrow diseases are multifaceted and depend on the specific condition.
These strategies aim to support the body’s ability to repair and regenerate bone marrow, bolster the immune system, and minimize the side effects of treatments like chemotherapy or radiation. Careful monitoring of nutrient intake is essential to ensure adequate levels of essential vitamins, minerals, and proteins.
Nutritional Requirements in Different Bone Marrow Disorders
Individuals with various bone marrow disorders exhibit different nutritional needs. For example, patients undergoing bone marrow transplantation often require higher calorie and protein intakes to support the healing process and counteract the side effects of the procedure, such as nausea and loss of appetite. Conversely, those with myelodysplastic syndromes (MDS) may experience anemia and require increased iron and vitamin B12 intake.
Similarly, patients with multiple myeloma may need adjustments to their diet to manage hypercalcemia and bone loss. These varying needs highlight the importance of individualized nutritional plans.
Nutritional Strategies for Managing Bone Marrow Diseases
Effective nutritional management of bone marrow diseases involves a multi-pronged approach. This includes dietary modifications to address specific nutrient deficiencies, nutritional supplementation to ensure adequate intake of essential nutrients, and medical nutrition therapy to manage complications associated with the disease and its treatment. For instance, patients undergoing chemotherapy may benefit from anti-nausea medications and small, frequent meals to manage treatment-related side effects.
Supplements such as omega-3 fatty acids may be recommended to reduce inflammation. Furthermore, close monitoring of weight and body composition provides valuable indicators of nutritional status and guides adjustments to the dietary plan.
Visual Representation: Bone Marrow Diseases and Nutritional Status
Imagine a graphic depicting two interconnected circles. One circle represents the “Bone Marrow Health” spectrum, ranging from healthy and vibrant (deep green) to severely compromised (dark grey). The other circle represents “Nutritional Status,” similarly graded from optimal (bright yellow) to severely deficient (dark red). Arrows connect points on each circle, illustrating the reciprocal relationship. For instance, a point representing severe aplastic anemia (dark grey in the Bone Marrow Health circle) is connected to a point showing significant nutrient deficiency (dark red in the Nutritional Status circle).
Conversely, a point representing healthy bone marrow (deep green) connects to a point illustrating optimal nutritional status (bright yellow). The graphic clearly demonstrates how compromised bone marrow health leads to nutritional deficiencies, and vice versa, emphasizing the crucial interplay between these two factors. Different disease states (e.g., leukemia, lymphoma, MDS) could be represented by different colored markers within the Bone Marrow Health circle, each with corresponding nutritional implications.
Popular Questions: Bone Marrow Nutrition Facts
Can I get bone marrow from a grocery store?
While bone marrow is a food source, it’s not commonly found in grocery stores in a readily prepared form. Its accessibility is limited.
Are there any risks associated with consuming bone marrow?
As with any food, there are potential risks. Concerns might include potential contamination or individual sensitivities. It’s advisable to source bone marrow from reputable sources and be aware of any personal allergies or intolerances.
How much bone marrow should I consume?
There isn’t a set recommended daily intake for bone marrow. Its consumption should be part of a balanced diet, and moderation is key.
Is bone marrow suitable for vegetarians or vegans?
No, bone marrow is not suitable for vegetarians or vegans as it is an animal product derived from bone.